Trump’s unmatched leverage over Netanyahu gives the prime minister little room to maneuver.
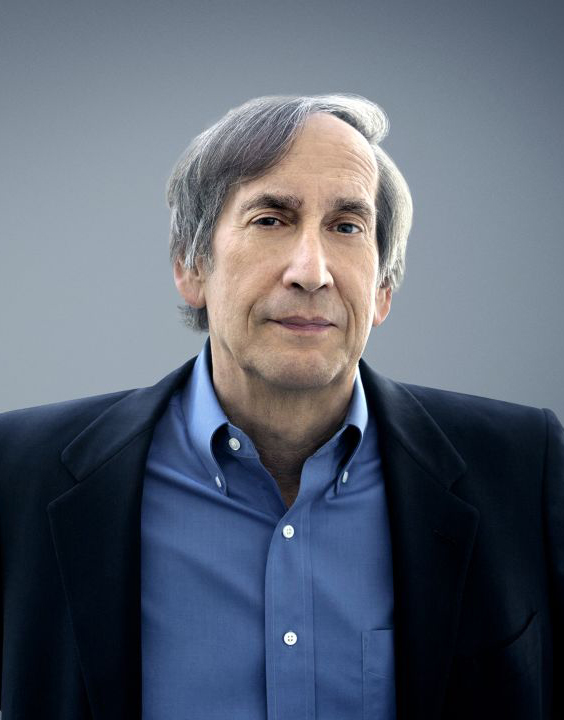
Aaron David Miller, Daniel C. Kurtzer
{
"authors": [
"Sara Halimah",
"Salmaan Keshavjee"
],
"type": "commentary",
"blog": "Emissary",
"centerAffiliationAll": "dc",
"centers": [
"Carnegie Endowment for International Peace"
],
"collections": [
"Rebuilding Gaza: The Human Dimension",
"Palestine/Israel Projects"
],
"englishNewsletterAll": "menaTransitions",
"nonEnglishNewsletterAll": "",
"primaryCenter": "Carnegie Endowment for International Peace",
"programAffiliation": "MEP",
"programs": [
"Middle East"
],
"projects": [],
"regions": [
"Palestine"
],
"topics": []
}
Kamal Adwan Hospital in northern Gaza in January. (Photo by Abood Abusalama/Middle East Images/AFP via Getty Images)
Healthcare delivery must be scaled up to meet demand, both inside Gaza and by transporting some patients elsewhere.
This piece is part of a series on the Gaza ceasefire.
After fifteen months of intense conflict, a fragile ceasefire has allowed those inside and outside the Gaza Strip to take stock of the scale of destruction. More than 90 percent of homes and schools have been destroyed, and the healthcare system has collapsed. Among the most pressing concerns is how to rebuild the health system to prevent further loss of life.
Those injured as a result of the conflict require immediate attention. The United Nations reported that up to ten children per day were losing one or both legs in Gaza, but despite a ceasefire, the number of amputations will continue to rise. Unexploded ordinances will pose a major threat as Palestinians return to their homes. The conflict has left behind patients suffering from extremely complex injuries, with no system in place to treat them, and limited rehabilitation services to address both physiotherapy needs and widespread mental health and psychosocial problems. Not only are these conditions burdening health systems, but they also are compounding and likely affecting almost every citizen in the Gaza Strip.
In addition, many with chronic conditions or who could not access care during the war remain in need. The absence of routine pregnancy care has affected thousands of Palestinian women and children. In the Gaza Strip, approximately 160 women give birth every day, most with little or no emergency obstetric care. Infectious diseases and malnutrition also must be prioritized and addressed.
The prolonged war has left a broken health system. According to the UN, only half of the thirty-six hospitals in Gaza are partially operational, and only 38 percent of primary healthcare facilities are functional. The supply of fuel, medical supplies, equipment, and deployment of specialist staff to sustain these facilities will be essential in the coming days and weeks. And as people return to what was once their homes as the ceasefire continues, health needs in different geographical areas will dramatically shift.
Invalid video URL
Given these circumstances, healthcare delivery must be scaled up to meet demand, both inside Gaza and by transporting some patients elsewhere. Inside Gaza, mobile health units can help provide immediate relief. Rather than focusing on single-disease treatment, these mobile units should be designed and deployed to provide comprehensive care directly to communities. These services include primary healthcare, emergency care, obstetric care, surgery, and rehabilitation. This bespoke model could provide needed flexibility and access while focusing on patient outcomes within Gaza.
Even with a variety of emergency solutions put into place, the burden of disease will outweigh the capacity of the health system, and many patients need care outside Gaza. However, the rate at which Israeli authorities issue permits leaves patients waiting, often in dire conditions. According to the UN, 2,500 children in Gaza are in urgent need of medical evacuation, but transporting them would take seven years at the current rate of approvals. Some of them will die waiting. Israel must allow critical patients to leave Gaza for lifesaving care, with no exceptions.
There are two distinct patient groups that should be transferred outside Gaza to help relieve the health system. One group requires relatively less complex management and should be moved to the West Bank. The second group needs complex management available only in surrounding countries, such as Jordan, Qatar, and Saudi Arabia, and should be permitted to move to those healthcare systems. Establishing a safe and accessible corridor for movement of these patients, without delays, will be a critical component to the response.
Another hurdle to restoring healthcare is staffing. Gaza’s healthcare workforce has been significantly depleted—according to the UN, more than 900 healthcare workers have been killed in the conflict. Others have been injured, detained, or fled abroad.
Efforts should begin immediately to rebuild Gaza’s healthcare workforce. Officials first must document the current healthcare workforce numbers and assess what it may be in a few months’ time, as some return to Gaza. The international community will be offering training across various disciplines. However, experience from past conflicts has highlighted that training should reflect the context and the level of materials and technology available in Gaza. It also should be accredited. In addition, local healthcare staff are often wooed away from the public sector because of relatively lucrative but short-term contracts offered by international organizations and the UN. The international community should recognize the detrimental impacts of this practice and instead support the public health sector in order to boost its long-term sustainability by supporting the payments of salaries. A central independent body should be established to oversee the training and retention of the public healthcare workforce.
Finally, international efforts to rebuild the health system must be intertwined with a local governance and coordination mechanism. This mechanism will be essential to prevent duplication and omissions in the provision of services and to avoid causing harm to the most vulnerable. Although the international community likely will deliver much of the healthcare in the immediate ceasefire period, developing a system in parallel that enables Palestinians to lead and deliver healthcare to their own population is essential.
By focusing on these priorities—comprehensive mobile health services, patient transfer, healthcare workforce, and local governance—Gaza can begin to rebuild its health system and provide the care its population urgently needs.
Read more in this series:
Carnegie does not take institutional positions on public policy issues; the views represented herein are those of the author(s) and do not necessarily reflect the views of Carnegie, its staff, or its trustees.
Trump’s unmatched leverage over Netanyahu gives the prime minister little room to maneuver.
Aaron David Miller, Daniel C. Kurtzer
Its role in facilitating security, governance, and other key components of the plan would help avoid the dangers of a permanent transitional administration.

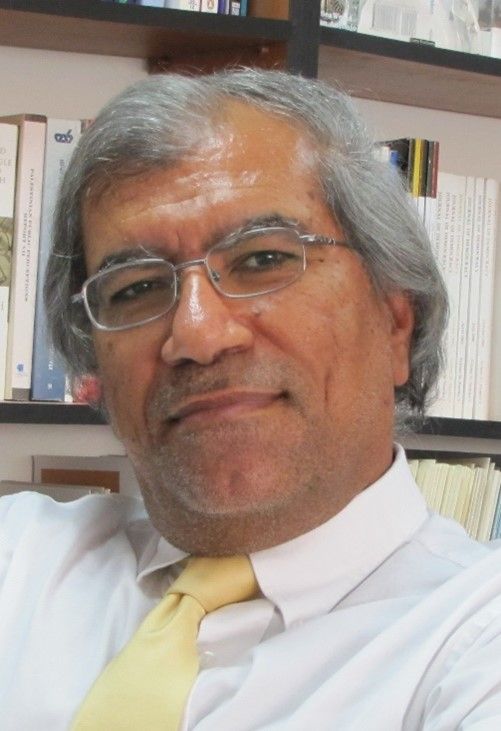
Amr Hamzawy
The factors that enabled the U.S. president to hammer out the initial success now doom its long-term prospects.

Charles H. Johnson, Frederic Wehrey
Trump has leverage over Netanyahu, and unlike his predecessors, he is not afraid to use it.
Daniel C. Kurtzer, Aaron David Miller
On paper, it may be good. But implementation and sustainability will be major hurdles.

Aaron David Miller, Natan Sachs, Khalil Shikaki